OUTBREAK OF MONKEYPOX
According to the US Centers for Disease Control and Prevention, the number of monkeypox cases worldwide has increased to over 7,500 in at least 57 nations. The monkeypox virus was formerly restricted to west and central Africa, but it is increasingly spreading to new nations—even those outside of Africa. The majority of new cases since early May have been documented in Europe, the US, and mainly among men who have sex with other men. Health officials are concerned that societal stigma would hinder efforts to track down and contain the disease because new cases are mostly affecting gay and bisexual males, as people may be less willing to disclose their symptoms or share their sexual history. Although monkeypox is often a mild viral illness, it can be dangerous or even fatal in extremely young children and immunocompromised individuals. It can be prevented with vaccines that are also used to immunize against smallpox because it is spread through close contact.
These vaccines are in short supply globally, and the WHO is collaborating with manufacturers to find a solution. The continent's top public health organization expressed the wish that wealthy nations would refrain from hoarding vaccines, as they did with COVID-19 inoculations, while monkeypox is endemic in 11 countries in Africa. In May, the UK reported a rare incidence of monkeypox, a virus related to smallpox. The initial UK case, which originated from a tourist in Nigeria, is now believed to be unrelated to the larger outbreak, but the UK rapidly reported a large number of additional cases. The virus has expanded to more than 4500 confirmed or suspected cases across at least 40 nations, including the US and Canada, with the UK having the greatest number of cases worldwide.
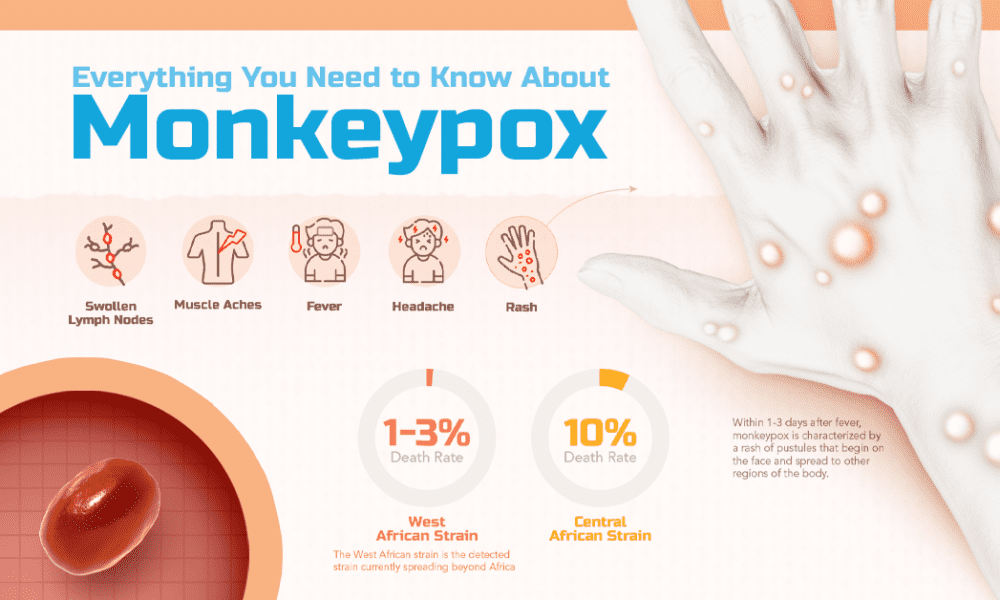
Textbook Flu-like symptoms are frequently the first signs of monkeypox. A few days later, you have a rash that typically starts on the face and spreads out after you have a fever, headache, muscle aches, and backaches. It has similarities to chickenpox. Starting to appear are flat, red spots that resemble pimples.
However, there have been numerous case reports of the current outbreak's symptoms, which have a rather wide range of appearances. Some people are experiencing no rash at all, while others are experiencing very mild rashes. Many times, instead of the rash beginning on the face, people only see it concentrated in the vaginal region. According to scientists, close contact is the main method of transmission for monkeypox.
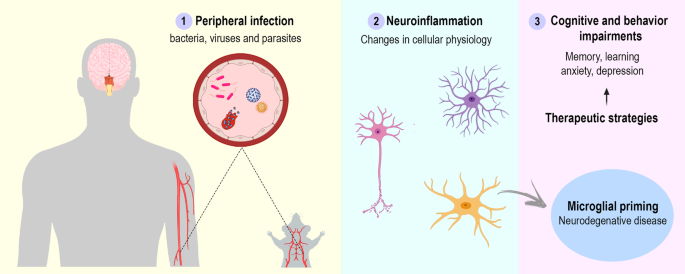
Previous studies have shown that respiratory droplets can transmit monkeypox virus particles over short distances, but it is unknown whether aerosols, which are much smaller airborne particles, can also transmit monkeypox. Therefore, contact with the pus-filled lesions that the disease generates has been linked to high viral levels, and this is thought to be the primary method of transmission. Compared to a virus that can be easily transferred through the air, such as COVID-19, monkeypox is significantly less contagious. However, it is fairly simple to catch if you are in close proximity to someone. According to US health officials, incidences of monkeypox are concentrated in particular areas. The CDC claims that at least part of the cases in the US are guys who are bisexual, gay, or who have intercourse with other men. Despite the fact that the virus can infect anyone, regardless of sexual orientation, infectious disease experts believe that some members of this community are at high risk for viral exposure and subsequent dissemination. This is the first time a recently emerging disease has surfaced and is concentrated in this population since the HIV epidemic of the 1980s.
One significant difference between now and then is that, in contrast to before, when public health officials responded slowly to the HIV epidemic, they are working extremely hard to reach out to any bisexual men now. They distribute information at Pride celebrations, for example. Push notifications are being sent on dating apps like Grinder. The majority of cases of monkeypox disappear without any medical intervention. However, certain antiviral medications and a vaccination created for smallpox also work to treat monkeypox. Bavarian Nordic of Denmark, the sole manufacturer of a monkeypox vaccine with a license, claimed it would meet demand. It functions exactly like a customary vaccine. Your immune system is strengthened. It boosts your immune system, putting you in a better position to combat the monkeypox infection you now have. The origin of the monkey in Monkeypox is the 1958 Danish discovery of monkeypox in laboratory monkeys. However, it is not believed that monkeys are the primary disease carrier or vector. It appears to be widely circulating among some rodents in the rain forests of the Congo Basin in central Africa, while scientists are unsure of whether the species is the primary carrier.
In the Democratic Republic of the Congo, a nine-year-old boy was the first person to contract the disease in 1970. There have been no reported fatalities from the current outbreak's about 4.5 thousand confirmed cases of monkeypox in nations where the virus is uncommon. In Nigeria, there has only ever been one fatality so far.